The Facts on Plantar Fasciitis:
Plantar Fasciitis 101
Plantar Fasciitis is the pain and inflammation at the point where the thin band of tissues called the plantar fascia connects your heel bone to your toes. This tissue helps support the bones of your arch and absorbs some of the strain you put on your feet, whether from running or other kinds of vigorous exercise.

DO I HAVE PLANTAR FASCIITIS?
The most common plantar fasciitis symptom is pain, which is normally felt at the heel and occurs where the plantar fascia attaches to the heel bone. The pain can be intense when getting out of bed in the morning or getting up from a stationary position. The pain often lessens when walking, but may be persistent.
Pain that is commonly intense when getting out of bed is a common sign of Plantar Fasciitis, a particular type of heel pain.
WHAT CAUSES PLANTAR FASCIITIS?
THEY NOTE, HOWEVER, SOME THINGS THAT CAN MAKE YOU MORE APT TO EXPERIENCE IT:
- Tight calf muscles, which can make it hard for you to flex your foot
- Being overweight, which can amplify the everyday shocks of moving
- Very high arches because the fascia are already under extra tension
- Repetitive impact activity like running, hiking or other sports
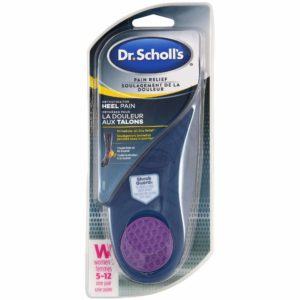
Shop Products for PLANTAR FASCIITIS
MANAGE PLANTAR FASCIITIS AND KEEP MOVING
Having plantar fasciitis is a painful experience that may even require surgery, so it’s important to talk with your doctor about your symptoms. He or she can help make sure you don’t have another condition and help you learn how to get the plantar fasciitis pain management plan you need, which may include
- Taking a break from activities that cause the pain
- Using ice for up to 20 minutes 3 to 4 times per day
- Medication as directed by a doctor
- Special exercises or therapies to help strengthen calf muscles or correct a problem with your gait
In addition, you may want to talk to your doctor about orthotic inserts or insoles from Dr. Scholl’s®, designed for added arch support
Not a medical diagnosis. For information purposes only. If you have diabetes, poor blood circulation, or fragile skin, or symptoms are severe or persist, consult your podiatrist or physician before using products.
†SOURCE: Kadakia, A. R., MD. (2010, June). Plantar Fasciitis and Bone Spurs-OrthoInfo – AAOS (S. J. Fischer MD & S. L. Haddad MD, Eds.). Retrieved January 25, 2017, from
http://orthoinfo.aaos.org/topic.cfm?topic=A00149